Gastroparesis can be a disabling condition, particularly when it severely impacts daily life and work ability. While it may not be explicitly listed as a disability by some organizations, the significant effects of its symptoms can qualify individuals for disability benefits.
What is Gastroparesis?
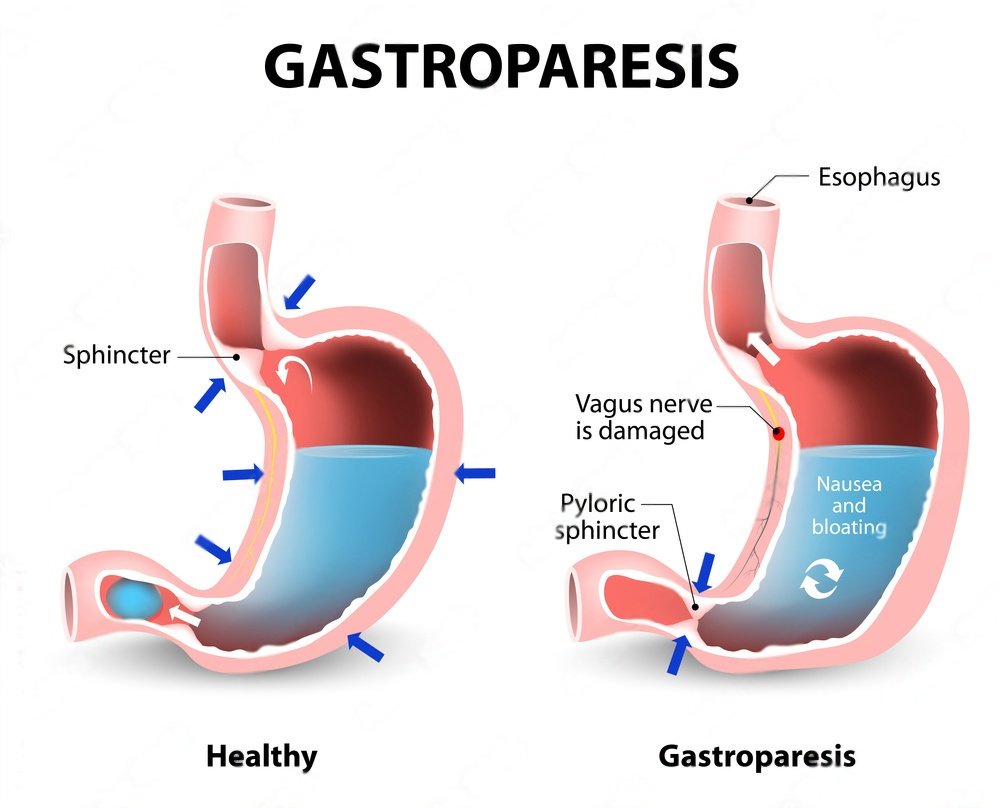
Gastroparesis is a condition where the stomach takes too long to empty its contents. This happens because the muscles in the stomach don’t work well. Normally, the stomach muscles contract to move food into the small intestine. In gastroparesis, these muscles don’t function properly, leading to slow or delayed digestion.
Symptoms of Gastroparesis:
People with gastroparesis might experience:
- Nausea
- Vomiting
- Feeling full quickly when eating
- Bloating
- Abdominal pain
- Weight loss or malnutrition
These symptoms can vary from mild to severe and can significantly impact daily life.
Causes of Gastroparesis:
Gastroparesis can be caused by several factors, including:
- Diabetes: High blood sugar levels can damage the vagus nerve, which controls stomach muscles.
- Surgery: Operations on the stomach or intestines can damage the vagus nerve.
- Medications: Certain drugs, like opioids or antidepressants, can slow gastric emptying.
- Other Conditions: Hypothyroidism, Parkinson’s disease, and certain autoimmune diseases.
Is Gastroparesis a Disability?
Whether gastroparesis is considered a disability depends on its severity and impact on an individual’s life. In some cases, gastroparesis can be so debilitating that it limits a person’s ability to work, perform daily activities, and maintain proper nutrition.
Legal Definitions and Disability Benefits:
- Social Security Disability Insurance (SSDI): In the United States, the Social Security Administration (SSA) does not list gastroparesis specifically as a disability. However, if gastroparesis significantly limits a person’s ability to work, they may qualify for SSDI. The SSA considers the severity of symptoms, how long they are expected to last, and how they impact daily living and work activities.
- Qualifying for Disability Benefits: To qualify for disability benefits, individuals must provide medical evidence, such as:
- Doctor’s diagnosis of gastroparesis
- Documentation of symptoms and their severity
- Treatment history and its effectiveness
- Impact on daily living and ability to work
Managing Gastroparesis
Management of gastroparesis involves several strategies to help reduce symptoms and improve quality of life:
- Dietary Changes:
- Eating smaller, more frequent meals
- Avoiding high-fat and high-fiber foods
- Consuming soft or liquid foods that are easier to digest
- Medications:
- Prokinetic agents to stimulate stomach muscle contractions
- Antiemetic drugs to reduce nausea and vomiting
- Medical Treatments:
- Feeding tubes for severe cases
- Gastric electrical stimulation (GES) to help control stomach muscles
- Lifestyle Modifications:
- Chewing food thoroughly
- Sitting upright during and after meals
- Avoiding lying down immediately after eating
Living with Gastroparesis:
Living with gastroparesis can be challenging, but with proper management, many people can lead a relatively normal life. Support from healthcare professionals, dietitians, and support groups can be invaluable. It’s essential to work closely with doctors to develop a personalized treatment plan that addresses specific symptoms and needs.
Conclusion:
Proper management through diet, medication, and lifestyle changes is crucial for improving quality of life. If you suspect you have gastroparesis or are struggling with its symptoms, consult a healthcare provider for a thorough evaluation and tailored treatment plan.
